The fastest selling out course in the UK!
ADS - Home of Master of Dental Teaching!
Bookings for October 2026 start
will be in May 2026!
"The most up to date comprehensive teaching in dentistry"
Cosmetic & Aesthetic Dentistry evolved over the last 20 years, and our programme updated continuously, so that it is still the best programme in the UK.
The Chris Orr Course is all about treating a whole mouth.
We teach building aesthetics and function into the treatment plan - regardless of whether it’s a veneer, crown, inlay-onlay, composite bonding or orthodontic case. By the end of one year, you are able to make a comprehensive assessment of all the potential risks for your cases – be they dental, periodontal, occlusal, or aesthetic – develop full mouth treatment plans, and explain this to the patient.
Using our tried and tested system, you will develop your clinical skills and confidence during the year. The first half of the programme will re-examine many of the techniques you will carry out on a day-to-day basis, to give a foundational skill set that is built upon in the second half of the year, as we consider the comprehensive treatment of the whole mouth as a functional and aesthetic entity.
EACH COURSE SESSION IS FOLLOWED UP WITH AN ONLINE RE-CAP WEBINAR TO SUMMARISE THE TOPICS COVERED
Click to see the Summary of the topics covered
Here is a summary of the topics covered…
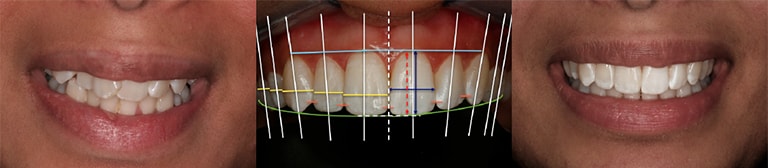
- Aesthetic treatment planning – "smile design"
- Digital Smile Design (DSD) protocol
- Aesthetic risk assessment & management
- Bleaching
- Shade matching
- Clinical photography
- Patient assessment & diagnosis
- Caries risk assessment & management
- Periodontal risk assessment & management
- Medico-legal aspects
- Patient communication – consent & expectation management
- Veneers
- All-ceramic crowns
- Inlays & onlays
- Anterior composite
- Class IV restorations
- Diastema closures
- Direct veneers
- Posterior composite
- Aesthetic posts
- Dentine & enamel bonding
- Occlusion: conformative & reorganised
- Occlusal risk assessment & management
- Occlusal appliances
- TMD in general practice
- Wear cases: Dental erosion & Bruxism - diagnosis and treatment
- Orthodontics
- Aesthetic bridges
- Implants in the aesthetic zone
- Aesthetic dentures
- Crown lengthening
- Pink composite & pink porcelain
- Pontic site development
- Failures and their management
- Gummy smiles
- Interdisciplinary treatment
Course Dates
| G1/Wednesday | G2/Thursday | G3/Friday | G4/Monday | G5/Tuesday | G6/Thursday | |
| 1-Aesthetic & functional treatment planning | 01/10/25 | 02/10/25 | 03/10/25 | 06/10/25 | 07/10/25 | 25/09/25 |
| 2-The diagnostic & consultation process | 29/10/25 | 30/10/25 | 31/10/25 | 03/11/25 | 04/11/25 | 06/11/25 |
| 3-Minimally invasive aesthetics | 26/11/25 | 27/11/25 | 28/11/25 | 01/12/25 | 02/12/25 | 04/12/25 |
| 4-Single anterior veneers & crowns; The restorative workflow | 07/01/26 | 08/01/26 | 09/01/26 | 12/01/26 | 13/01/26 | 15/01/26 |
| 5-Posterior aesthetic restorations | 04/02/26 | 05/02/26 | 06/02/26 | 09/02/26 | 10/02/26 | 12/02/26 |
| 6-Advanced anterior composite restorations | 04/03/26 | 05/03/26 | 06/03/26 | 09/03/26 | 10/03/26 | 12/03/26 |
| 7-Advanced veneer cases; Ceramics update | 08/04/26 | 09/04/26 | 10/04/26 | 13/04/26 | 14/04/26 | 16/04/26 |
| 8-Aesthetic & Function: Tooth wear & Occlusal management | 06/05/26 | 07/05/26 | 08/05/26 | 11/05/26 | 12/05/26 | 14/05/26 |
| 9-Specialist interfaces in restorative dentistry | 03/06/26 | 04/06/26 | 05/06/26 | 08/06/26 | 09/06/26 | 11/06/26 |
| 10-Aesthetic tooth replacement | 01/07/26 | 02/07/26 | 03/07/26 | 06/07/26 | 07/07/26 | 09/07/26 |
| 11-Planning & delivering comprehensive dentistry | 29/07/26 | 30/07/26 | 24/07/26 | 27/07/26 | 04/08/26 | 06/08/26 |
| 12-Aftercare, Repairs & Maintenance; Managing failures | 02/09/26 | 03/09/26 | 04/09/26 | 07/09/26 | 08/09/26 | 10/09/26 |
Detailed Course Programme
Overall learning objectives
After completion of the whole course, participants should have gained knowledge & understanding of the following:
- current concepts and techniques in dentistry;
- current materials and techniques for contemporary restorations, with an emphasis on minimising invasiveness in the provision of these restorations;
- a structured approach to the diagnosis, planning and execution of aesthetically-driven treatment plans;
- the role of orthodontics, periodontics and other specialities in developing and delivering the treatment plan;
- a structured approach to patient communication to maximise patient involvement and minimise risk in planning and delivering treatment;
- the use of digital smile design as a way of planning and communicating treatment plan
This knowledge is built throughout the year, via the structured programme.
This is not a modular programme – there are many recurring themes throughout the year, so the material covered in the middle of the year builds on what was covered at the start. In the same way, the material at the end of the year builds on what was covered before.
This is why it is crucial that if you manage to book yourself on the programme, you should block the course dates in your diary in order to not miss a session.

Smile design, Occlusal foundations
Lectures & Literature discussions:
Aesthetic treatment planning:
- facial aesthetics
- facial landmarks in aesthetic treatment planning
- smile analysis & visualisation of the aesthetic outcome of treatment
- “smile design”: aesthetic dental treatment planning
- why smile design is not just about veneer cases
- traditional and digital tools for smile design
Functional treatment planning:
- occlusal foundations for restorative dentistry and aesthetic orthodontics
- assessment of the occlusal system
- assessing the impact of the treatment plan on the patient’s occlusion
- rules for occlusal management in everyday dentistry
- occlusal case complexity assessment: conformative vs. reorganised approaches
Overview of different approaches to aesthetic & functional treatment planning:
- DSD, FGTP (EFSB), Dawson, Swiss 3-step
Evidence-based dentistry:
- separating scientific journals from clinical newspapers
- Implementing research findings into daily practice
Practical: Smile Design exercises
Learning objectives
After the Day 1 programme, participants should have gained the following:
- An appreciation of the changes in dental care in the US and the UK over the last 20 years, and the impact this will have on the future of care in this country;
- An overview of the process of comprehensive dental treatment planning;
- An understanding of the art and science of facial and dental aesthetics and to learn a structured, logical approach to aesthetic dental treatment planning (“smile design”).
- An understanding of how some of the rigid classical concepts of treatment planning have given way to modern, more flexible approaches;
- An understanding of the interplay between the different factors in smile design;
- An understanding of traditional and digital tools used in the smile design process;
- An understanding of the foundational functional concepts in the healthy occlusal system;
- A system of assessing case complexity based on the impact of the treatment plan on the patient’s occlusion;

consultation skills: patient assessment, photography, consent, fee setting, TREATMENT PRESENTATION
- Internal vs external marketing to identify interested patients
- Structured consultations for new & existing patients
- Consultation technique: communication skills
Comprehensive patient assessment
- what an NHS exam covers and what it does not
- risk management via a comprehensive exam
- aesthetic consultation structure: 1 visit vs 2 visit
- essential vs. case-specific information
- Discussing elective treatment with your patients – making a ‘problem list’
- Co-diagnosis for enhanced communication in the consultation
- Developing the treatment plan
- Fee setting
- Case presentation
- Consent to treatment / other medico-legal aspects
Clinical photography
- record-keeping and beyond
- choosing the right camera for you
- photographic technique for quality, reproducible images
- standardised photographic views for records and treatment planning
- which additional views to take for DSD, orthodontic cases or for shade matching
Photography practical
- all participants to be photographer/assistant/patient
- view and critically evaluate each others’ results at end of session
Learning objectives
After the Day 2 programme, participants should have gained the following:
- A systematic way to record clinical information prior to aesthetic treatment planning;
- Information on using a structured approach to aesthetic consultations to ensure good communication between dentist and patient;
- An appreciation of the different kinds of interpersonal communication and how they affect the message we try to get across;
- An understanding of the source of common medico-legal complications of aesthetic and cosmetic treatment;
- Introduction to a reproducible scheme for clinical photography to aid record keeping and self-evaluation of treatment outcomes;
- An appreciation of how to ensure valid consent is given;
- An understanding of different strategies for fee setting for small and larger courses of treatment;
- Knowledge of how to discuss treatment plans with patients, present treatment and discuss fees.

adhesion / bonding, micro-abrasion, resin infiltration, bleaching
Adhesion to tooth tissue:
- understanding the bonding “systems”
- historical approaches vs. current practice
- total etch, self-etch & selective etch
- immediate dentine sealing
- adhesion to other substrates
Resin infiltration for smooth-surface caries and white spot discolouration
Microabrasion & Mega-abrasion
Cosmetic (re)contouring
Simple orthodontics as a means of minimising intervention
- Orthodontic components of the patient assessment
- Market overview:
- removable appliances, clear aligners, fixed appliances, branded alignment products
- what can (and cannot) be easily achieved with the different orthodontic “systems”
- Choosing the treatment modality: restorative vs. orthodontics
Bleaching:
- home, in-surgery, “assisted”, non-vital methods
- complex bleaching: single dark teeth, tetracycline staining, fluorosis
- tray fabrication
- over-the-counter products
- legal update on bleaching
- marketing whitening within the practice
- “therapeutic aesthetics”: anti-caries use of bleaching products
Hands on:
- Micro-abrasion
- Resin infiltration
Learning objectives
After the Day 3 programme, participants should have gained the following:
- An understanding of current products available for adhesion (“bonding”) to tooth tissue and other substrates;
- Knowledge of appropriate product selection for different scenarios to optimise adhesion;
- An appreciation of the importance of substrate control;
- An understanding of non-invasive and minimally invasive techniques for management of anterior aesthetic problems;
- Knowledge of current concepts of resin infiltration and micro-abrasion;
- An understanding of when to use cosmetic contouring to achieve a more ideal embrasure form;
- An introduction to introducing adult orthodontic treatment into general dental practice;
- An understanding of orthodontic assessment in the adult patient;
- An appreciation for how simple orthodontics can reduce or eliminate the need for tooth preparations;
- An overview of different systems for tooth whitening and an appreciation of when to use which one;
- An introduction to the skills of patient expectation management using bleaching as the treatment.

shade matching, tooth preparations, impressions, temporaries
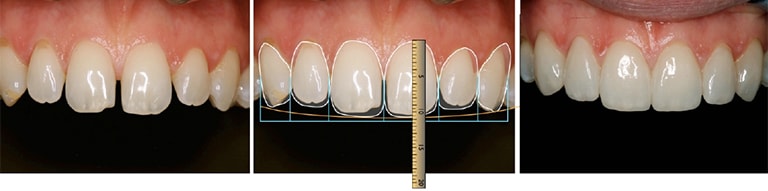
Case workflow:
- integrating the aesthetically-driven workflow into routine anterior cases
- step-by-step execution of the treatment plan
- use of diagnostic wax-ups, matrices and preparation stents
- minimizing intervention for veneer cases using the bonded mockup (APR/APT “Gurel”) technique
- luting/cementation & finishing; post treatment review & maintenance
- impressions, temporisation & lab communications
- fitting & finishing
- post treatment review & maintenance
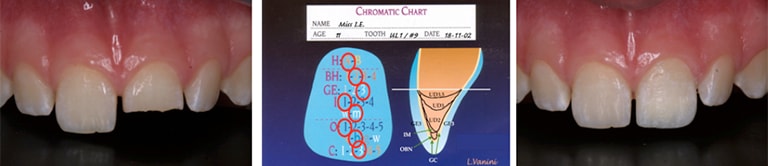
Colour in dentistry:
- the dimensions of colour
- visual perception of colour
- dental tissues and colour perception
Shade matching
- the scientific basis of colour measurement
- the problem of matching single restorations
- better use of shade guides
- impact of lighting conditions on shade matching
- seeing & mapping internal colour effects
- computer-assisted shade matching
- laboratory communication of colour information
Ceramics
- overview of available products; comparison of clinical & aesthetic properties
- tooth preparations for veneer & all-ceramic/traditional crowns
Hands on
- Colour mapping & shade taking exercises
- Veneer preparation using APR-APT technique to minimise preparations
- Impression taking
- Chairside temporisation techniques
Learning objectives
After the Day 4 programme, participants should have gained the following:
- Knowledge of a visit-by-visit clinical workflow for indirect restorations, from initial appointment to final review;
- A working knowledge of the inter-relationship of hue, value, chroma and other factors in colour matching for restorative dentistry;
- An understanding of the importance of correct lighting for accurate shade selection and colour mapping;
- A system for evaluating, recording and communicating internal colour effects in the natural dentition;
- A reliable method for shade selection;
- An appreciation of the differences in physical, aesthetic and biomechanical properties of current all-ceramic restorations;
- An understanding of clinical ceramic material selection, preparation design and luting cement selection based on these properties.
- Knowledge of different preparation techniques for veneer cases and an understanding of how tooth preparations can be influenced by the desired outcome and the material chosen;
- Knowledge of chairside direct temporisation techniques;
- Understanding of cementation techniques.

posterior composite, LAYERING vs. bulk fill; inlays, onlays
Modern approaches to caries diagnosis, risk assessment & control
The range of posterior restorations:
- direct restorations, inlays, onlays, endo crowns, onlay crowns, full crowns
Caries management
- current concepts of diagnosis & risk asessment
- minimising intervention in caries treatment: prevention of extension
Posterior direct restorations:
- repeat interventions – caries vs electively-driven
- the amalgam debate: what to say to patients
- layering vs. bulk fill techniques
- creating internal colour effects: fissure stains & hypoplastic areas
- finishing, polishing & texturing
Restoration of endodontically treated teeth:
- aesthetic posts
- current concepts of structure & function for post-retained crowns
- ferrule effect
- discoloured teeth: ditch preps & localised opaquing
- decision-making on endodontic re-treatment before post placement
Indirect restorations
- ceramic vs. composite
- partial coverage vs. full coverage
- onlays as a conservative alternative to crowns
- core buildups: why & when?
- restoration of the endodontically treated posterior tooth
Hands on
- Posterior direct composite – layering & bulk fill
- Direct post placement & core buildup
Learning objectives
After the Day 5 programme, participants should have gained the following:
- An appreciation of the range of posterior restorations possible with modern restorative materials;
- Knowledge of current approaches to caries diagnosis and managementbased on risk assessment
- An understanding of the differences between treating primary caries and replacement of old restorations with these materials;
- A better understanding of the potential problems that can arise in the placement of direct restorations in class I & II cavities and how to limit these problems;
- To learn when direct posterior restorations are inappropriate and to understand appropriate alternative treatments;
- An understanding of the different preparations and materials for indirect posterior restorations and the strengths and weaknesses thereof;
- A working knowledge of how adhesive dentistry can allow for more conservative approaches to treatment with both direct and indirect restorations;
- Understanding of when to use aesthetic posts and core build-ups on posterior teeth.
anterior composite layering, class IVs, diastema closure, peg laterals
Composite resins:
- physical vs. optical properties
- concepts of shading: Vita vs. non-Vita
Class III & V restorations
- material selection for different cavity configurations
- marginal bevels
Class IV restorations & direct resin veneers:
- layering techniques for anterior direct restorations
- marginal bevels
- colour mapping for large composite restorations
- minimal intervention with direct composite
- use of wax-ups and layering matrices
- creating internal effects: mamelons, incisal translucency & white spots
- finishing, polishing & texturing
- using indices for large composite resin buildups
Hands on:
- Colour mapping for composite restorations
- Anterior direct composite – building the colour map,
- Finishing, texturing, polishing
- Diastema closure
- Class IV restoration
Learning objectives
After the Day 6 programme, participants should have gained the following:
- An introduction to the materials science behind modern composite resins and how their physical and optical properties affect clinical usage;
- To learn current approaches to anterior composite layering techniques;
- To appreciate the importance of relative translucency and opacity in building restorations that mimic nature;
- To practice polishing and finishing techniques that will enhance the aesthetic appearance of a direct restoration;
- To recognise the limitations inherent to composite resin;
- To learn when direct anterior restorations are inappropriate and appropriate alternative treatments.

complex veneer cases, preparation design, Minimising invasiveness
Treatment planning
- aesthetic and functional planning for larger anterior veneer cases
Complex cosmetic cases
- dark teeth, diastemas, disguising gingival recession
- ultra minimally-invasive restorative treatment spacing and recession
- advanced use of APR-APT technique
Ceramics
- the ceramic marketplace: feldspathic, eMax, zirconia, Suprinity, Enamic & the others
- variations in material selection & preparation based on the clinical scenario
- rationale for material selection for different situations
- managing dark teeth / metal posts under ceramic restorations
Hands on
- preparation of a complex case for diastema closure & recession
Learning objectives
After the Day 7 programme, participants should have gained the following:
- Further understanding of how preparation design affects the final shape of the restorations, building on material covered in day 4;
- Knowledge of when to extend preparations interproximally, and how much preparation is appropriate;
- A more detailed understanding of techniques available to minimise tooth preparation;
- A more detailed understanding of ceramic material selection for challenging clinical situations
- An understanding of different impression materials and techniques and when each of them is appropriate.

occlusion, tooth wear, Dahl concept, facebows, articulators
Tooth wear:
- effective diagnosis & aetiologically-driven treatment
- current guidelines for erosion screening & management
- use of the “Dahl concept” to simplify treatment of wear cases
- minimising intervention in wear cases
- current concepts of bruxism management
Occlusion II:
- philosophies of occlusion
- articulators & facebows: why, which and when?
- the importance of anterior guidance
- occlusal risk management for more complex cases
- reorganisation for predictable dentistry – what, when, why and how to do it
- CR Bite records
- assessment of aesthetics, phonetics and function via long term provisionalisation
TMJ assessment:
- TMD screening examination
- Load testing
Opening vertical dimension:
- when, why & how
- to Dahl or not to Dahl?
Hands on:
- facebow practical
- leaf gauge practical
Learning objectives
After the Day 8 programme, participants should have gained the following:
- Understanding of how to diagnose and plan treatment for tooth wear cases;
- Understanding of risk management for tooth wear cases.
- A deeper understanding of the interaction between the aesthetic and functional aspects of a treatment plan;
- An understanding of how to avoid unplanned alterations to the patient’s anterior guidance;
- Knowledge of the clinical stages in treating complex aesthetic cases;
- An understanding of the different articulators available, and which to use for most cases;
- Knowledge of facebow transfer systems and how the information is transferred to the articulator in the laboratory;
- An understanding of the difference between conformative and re-organised approaches to occlusion;
- Knowledge of when a re-organised approach is appropriate and the bite records that are needed;
interdisciplinary cases, digital TREATMENT PLANNING
Interdisciplinary treatment:
- the role of orthodontist, periodontist, maxillofacial surgeon, endodontist, implant surgeon and non-surgical facial aesthetics practitioner
Management of periodontal disease in general practice
- screening examination (BPE)
- detailed examination & treatment guided by the BPE examination
- primary vs. secondary care: what to treat, what to refer
- “prognostication” of periodontally questionable teeth
Aesthetic soft tissue management:
- cosmetic aspects of periodontics
- gingival biotypes & the dento-gingival complex
- periodontal plastic surgery: gingivectomy, crown lengthening, root coverage
- when to perform a gingivectomy vs. osseous crown lengthening
- working with a periodontist for the procedures you do not wish to perform
- how orthodontics can help with aesthetic soft tissue management
- prosthetic approaches: pink composite, pink porcelain, gingival masks
The orthodontic-restorative interface
Gummy smiles:
- diagnosis & interdisciplinary management
Digital treatment planning for team communication
-
2-dimensional digital treatment planning
-
Introduction to 3-D digital smile design
Hands on
- 2-dimensional digital treatment planning: demonstration & practical
Learning objectives
After the Day 9 programme, participants should have gained the following:
- An understanding of gingival architecture and its normal variants;
- An update on current concepts of periodontal disease screening and management within general practice;
- An understanding of the concept of biologic width and its importance in soft tissue management;
- An understanding of the consequences of violating the normal gingival architecture with restorations;
- Knowledge of different techniques to enhance soft tissue aesthetics, both surgical and prosthodontic.
- An understanding of the options for diagnosis and interdisciplinary management of gummy smile cases;
- A working knowledge of the digital and clinical tools and their role in the consent and communication process;
- To introduce Apple Keynote as a means of providing images generated by the 2D Digital treatment planning process
- To introduce 2-dimensional digital smile design concepts & workflows

bridges, implants, dentures, treatment planning
Aesthetic tooth replacement
- The decision process for replacement of missing teeth
Evidence-based bridge design:
- the pros and cons of fixed-fixed, fixed-moveable, cantilever, adhesive designs
- common design flaws
- strategies for bridges involving compromised teeth
- aesthetic aspects: all-ceramic bridges vs. traditional PFM
Demystifying implants
- overview of the treatment workflow, surgical and restorative
- patient selection & assessment
- communication with the implant surgeon to ensure optimal implant positioning
- aesthetic considerations for anterior and posterior implants
- soft tissue management around dental implants
Aesthetic soft tissue management for tooth replacement:
- ovate pontic site creation
- papillary management around replacement teeth
- peri-implant soft tissue aesthetics
Aesthetic dentures
- aesthetic improvements for denture bases
- aesthetic denture teeth: customised setups for natural aesthetics
- design enhancements to partial dentures to improve aesthetic and longevity
- strategies for ‘claspless’ dentures: workflow to combine crowns with dentures
- historical concepts (milled crowns, stable-base dentures), precision attachments, Konus/telescopic crowns, overdentures on teeth & implants
Learning objectives
After Day 10 programme, participants should have gained the following:
- A systematic approach to treatment planning for replacement of missing teeth;
- Understanding of the importance of short, medium and long-term planning when replacing missing teeth;
- A working knowledge of the balance between aesthetics and conservation when planning tooth replacement;
- An overview of current materials and techniques for bridges, dentures and implant-supported restorations;
- An understanding of the clinical workflow for the placement of bridges, dentures and implant-supported restorations;
- An understanding of how aesthetic considerations can affect these processes;
- Understanding of the various periodontal and prosthodontic approaches to soft tissue management in relation to the replacement of missing teeth;
- Knowledge of when to apply the various techniques for the optimum result.

full mouth rehabilitations, treatment planning
The comprehensive approach to treatment:
- occlusal re-organisation as part of a larger treatment plan
Simplifying diagnosis and treatment planning for full mouth cases
TMD symptoms
- differential diagnosis and management
- the role of appliance therapy in restorative dentistry
Questionable teeth
- discussing the options and involving the patient in decision-making
Workflow for full-mouth cases
- long-term provisionalisation
- optimising aesthetics, function and phonetics
- clinical & laboratory sequence for transition to final restorations
Psychologically challenging patients
- recognising and managing “difficult” patients
Interdisciplinary aspects of comprehensive care
- building your interdisciplinary team
- interdisciplinary team diagnosis & treatment planning
- managing communication within the team
- transitioning patients within the team during treatment
Practical
- Treatment planning, sequencing & fee setting
Learning objectives
After the Day 11 programme, participants should have gained the following:
- When a full-mouth approach to treatment is appropriate
- Knowledge of when and how to reorganise the occlusion;
- Understanding when appliance therapy is appropriate within the treatment plan;
- Understanding of the components of the occlusion that should be incorporated into treatment planning for large cases;
- An understanding of the stages of treatment and time involved for each stage, so that patient expectations can be managed and appropriate fees set.
- An understanding of the roles of different specialties in the treatment process;
- An understanding of how complex interdisciplinary cases should be sequenced and delivered;
- Knowledge of different personality traits and how these can affect dentist-patient interactions;
- Understanding of an effective strategy to manage psychologically challenging patients

recognising & managing failures, treatment planning
Aftercare & Maintenance
Repairing restorations to extend their clinical longevity
Failures: diagnosis, prevention & management
Troubleshooting / repairs
Learning from failures
Practical:
- Quickfire treatment planning & fee calculation
- Presentation of your cases
Learning objectives
After the Day 12 programme, participants should have gained the following:
- Knowledge of maintenance procedures and the role of the hygienist in the aesthetic practice.
- Understanding of the causes of failure in aesthetic treatments;
- Knowledge of the reported success and survival rates for different treatments from the literature;
- Knowledge of useful solutions to common problems;
- An understanding of the techniques available to repair existing restorations;
- An understanding of how to manage difficult situations and resolving them to everyone’s satisfaction.
The course sessions are held at our custom-built postgraduate education facility, close to London Bridge station.
Advanced Dental Seminars11a Bell Yard Mews
Bermondsey Street
London SE1 3TN
Each day, the morning lecture starts at 9.15am and we will finish at around 5.00pm.
Participants who manage to book themselves on the programme receive a detailed Welcome booklet with info about the venue, local neighbourhood and possible places to stay overnight as over 70% of our participants travel to us from all parts of UK and Europe.
All bookings are done online through our website.
Course sessions cost £750.00 + VAT per day. There are 12 sessions on the programme.
Payments are done by setting up a direct debit payment on our website during the booking.
Initial booking fee is £900.00 ( £750.00 + 150.00 (VAT) ), which is deducted from the total payment
The remaining fee for 11 days is divided into 6 equal amounts to make it easily manageable sum for delegates and payments of £1650.00, including VAT, is taken out by DD, every other month, starting in September each year.
Tea and coffee are provided at appropriate intervals throughout the day.
A buffet lunch is provided. If you prefer to go out, there are numerous establishments offering a full range of culinary options just a few minutes’ walk away from our venue.
Please note that currently we are not able to cater for specific dietary requirements. Special care is given to provide a wide selection of options.
Q: Does the ADS Year Course give a level 7 PGCert / PGDip?
A: This is available as a separate follow on programme, once you have completed the initial Year Course. Over the years, our delegates have told us that they preferred to simply focus on their everyday practice for their patients and not have the added stress of completing assignments or preparing for exams. This takes the pressure off the learning and allows delegates to focus on implementing the teaching in their own time.
Because there are no exams or assessments, the ADS Year Course simply provides a completion certificate and CPD hours at the end of the year.
However, as we already have the accreditation for credit towards a Level 7 Postgraduate Diploma, delegates who have finished the ADS Year Course, will have the opportunity to sign up for the ADS Diploma programme, as a follow up, to further refine their skills and gain a PGDip.
Q: What is the ADS PGDiploma programme?
A: The ADS PGDip in Cosmetic & Aesthetic Restorative Dental Sciences (to give its full title) is designed to allow ADS Alumni to receive a PGDip qualification. This follow up programme will reinforce the key skills learned during the Year Course through revisions and updates.
More importantly, ADS PGDip qualification includes the curriculum of our former Advanced Occlusion and Complex Treatment Planning programme, which we used to run as the follow on programme.
In common with all qualifications of this level, there will be some assessments and clinical case presentations. The programme will support delegates through completion of the assignments and preparing the clinical case presentations necessary for the award of the Level 7 qualification.
Q: Why payment only with Direct Debit?
A: We wanted to make the programme more accessible financially to suit everyone’s budget. This is why 12 sessions worth of fees are taken in 7 parts (including the initial booking fee) to make it manageable sums to delegates. DD is set on a secure platform on our site and creates a straightforward payment method for both the delegate and us. Delegates have easy access to their payment info by logging into their dashboard on our site after the booking.
Q: What happens if I miss a day?
A: You will receive the reading material and handouts so that you can see what was covered. You will still be expected to pay for that session even if you do not attend. If the session is repeated again in following year's course, you may attend this session at no charge. We allow up to two sessions to be carried over to the next run of the course in this manner, provided that the sessions are repeated in the same format. We are not under any obligation to offer a missed session in the following year if the course is not run in the same format.
Q: Is there an examination at the end of the course? Do I have to present any cases?
A: No, there is no formal examination at the end of the course ADS Year Course. On the last day there is an optional case presentation by the participants as it is a nice way of rounding off the year, but it is not compulsory to present a case.
Q: Do we get a certificate at the end of the year?
A: All delegates, who attend a minimum of 10 sessions during their course year, receive a post-graduate dental certificate in Cosmetic Dentistry & Aesthetic Restorative Dentistry from ADS to prove their attendance on the programme.
Q: Do I have to bring patients for treatment?
A: No, there is no live patient treatment in this programme.
Q: What if I decide to withdraw from the course after booking my place?
A: Our reservation policy allows you to cancel your booking within the first 14 days of the online booking on ADS website and you will receive a full refund of the initial payment. No refunds are given after the 14 days for any cancellations.
All cancellations must be made in writing to info@advancedentalseminars.com email address in order to receive the full refund within the first 14 days of the booking.
FURTHER INFORMATION
Please check FAQ tab above to find out more about the programme.
If you still have Qs to ask, the best way to contact ADS Team is by email on info@advanceddentalseminars.com
Following our IG or FB pages is the best way for being notified of announcements of bookings.
Please note, Advanced Dental Seminars reserves the right to refuse or cancel a booking.
